Genetic-abnormality
Treatments
- PGD
- PGS
- Sperm DNA Fragmentation
- Donor Program
- Endometrial Receptivity Array
- Karyotyping
PGD - Pre-implantation Genetic Diagnosis
What is it?
Pre-implantation Genetic Diagnosis is genetic screening technique which allows an expert to examine the genetic composition of a pre-embryo before it is transferred to the patient’s uterus so that, transmission of hereditary disorders into next generation can be avoided.
Why is it recommended?
A normal human genetic code consists of 23 pairs of chromosomes, and each of the chromosomes may contain hundreds of genes. This genetic material is inherited from gametic cells of both mother and father. The combination of these genes creates the character blueprint for the offspring. Unfortunately, the process may not always work seamlessly. Disorders in the chromosomes or particular gene lead to complications in pregnancy or miscarriage or serious genetic diseases. PGD can help in identification of the issues well before the pregnancy occurs.
In an IVF cycle, the embryos are selected using visual criteria: the embryo or embryos that look healthy are chosen for transfer. Sometimes, a visual inspection is not enough. Some serious genetic abnormalities are invisible to the eye. This is where PGD can be used. Following hereditary abnormalities can be identified with PGD:
- Turner’s syndrome.
- Klinefelter’s syndrome.
- Translocation which can cause miscarriages or some forms of leukemia or cancer.
- Cystic fibrosis.
- Tay-Sachs disease.
- Duchenne muscular dystrophy.
- Sickle-cell anemia.
When is it recommended?
PGD can be recommended in following conditions:
- Women age 35 and older because there is a concern about the genetic quality of their eggs.
- Women experiencing recurrent, unexplained pregnancy loss.
- Women with more than one failed fertility treatment.
- Carriers of sex-linked disorders – they can choose gender determination to prevent sex-linked disease.
- Carriers of single gene disorders.
- Couples with family history of inherited disease.
- Those with chromosomal disorders.
What are the advantages?
- Avoids the need for amniocentesis (with a needle and syringe, some amniotic fluid from around the embryo is drawn for pre-natal examination) which be an uncomfortable technique and involves some risk.
- Enables the selection and implantation of healthy pre-embryo resulting into better chances of pregnancy and lower possibility of miscarriage.
- With proper screening fewer embryos are used for transfer thus, minimizing possibility of multiple births.
PGS - Pre-implantation Genetic Screening
What is it?
It is the genetic study of embryo produced during IVF treatment & can help in having a healthy baby. The technique is helpful to identify embryos with the correct number of chromosomes for successful fertility treatment. PGS is performed on the embryo before it is transferred. This allows the identification & transfer of embryos free from any hereditary abnormalities.
When is it recommended?
It is recommended under following conditions:
- If the female partner is more than 35 years.
- The female has suffered 2 or more miscarriages.
- There is history of previous IVF failures.
- Infertility is due to some male factor.
What are the advantages?
- Reduced miscarriage rates.
- Higher pregnancy rate per transfer.
- Greater chances of having a healthy baby.
Sperm DNA Fragmentation
What is it?
It is a test performed with fresh ejaculate received from the patient. This is an effective method for measuring DNA damage in thousands of sperm in the ejaculate. It measures the susceptibility of sperm DNA to denaturation process such as exposure to heat or acids. After this exposure sperms are stained with a fluorescent probe (dye) that interacts with the DNA molecule. Then quantitative analysis made about sperms with fragmented DNA.
How is it done?

- Freshly collected ejaculate is subjected to treatment with certain agents like acids or heat.
- The sample is then stained appropriately and observed under microscope to find out the proportion of sperms with fragmented and non-fragmented DNA.
- On the basis of this proportion suitability of the semen sample for IVF, ICSI or IMSI can be decided.
How can it be treated?
- Damage caused to sperms by oxidative stress can be treated with change in lifestyle and appropriate diet for avoiding oxidative stress.
- If the damage is due to infection, treatment of infection with antibiotics can be beneficial in reducing sperm DNA damage.
- Varicocoele is one of the commonly known causes of male infertility and it is associated with sperm DNA damage. Treating varicocoele can improve sperm DNA integrity.
- Generally DNA damage occurs at the post-testicular (i.e. in the ejaculate) level and testicular sperms are likely to have healthier DNA integrity than ejaculated sperms. ICSI may be an effective treatment than IVF for sperm with high DNA fragmentation.
Donor Program
What is it?
When the patient couples have problems in conceiving and if the problem is found in the quality / quantity of germ cells (Gametes), oocytes or spermatozoa or embryos are collected from suitable donor and used for ART.
When is it recommended?
It is recommended in following situations.
- If the female partner is not able to produce oocytes suitable for fertilization, oocytes can be received from a suitable (depending on blood group and other body features) donor female.
- If semen sample of the male partner does not contain any sperms (Azoospermea) or adequate number of sperms (Oligospermia) or properly motile sperms (Asthanospermea) or morphologically abnormal (Teratospermea), sperms are received from a suitable donor male.
- If gametes from both the partners are not suitable for fertilization and further implantation, preformed embryos formed by fusion of gametes from appropriate male and female donor are taken used for ART.
How is it done?
- When oocyte donation program is to be conducted, the healthy donor female is contacted and is given suitable hormone therapy for release for oocytes. These eggs can be used for IVF and then can be transferred into uterus of recipient who is also on hormone therapy.
- In sperm donor program, healthy and suitable male is contacted and his semen sample is collected on the same day when IVF is to be performed. The eggs collected from female partner are fertilized in vitro and used for fertilizing the oocytes.
- For embryo donation program, oocytes from suitable healthy female (who is on hormone therapy) are collected. On the same day, semen is also collected either from the concerned male partner or donor and is used for IVF. After fertilization, the embryo development is allowed to proceed for three or five days depending upon hormonal status of the recipient. The embryo in 8 cell stage or Blastocyst stage is used for transfer into recipient female’s uterus.
Endometrial Receptivity Array
What is it?
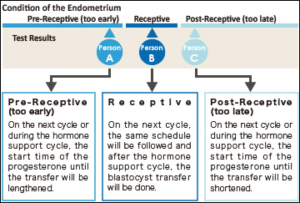 The term ERA stands for Endometrial Receptivity Analysis or Array. In this test, a small sample tissue from endometrial lining (innermost layer of Uterus) is used for evaluating whether the Uterus is ready for implantation of embryo or not.
The term ERA stands for Endometrial Receptivity Analysis or Array. In this test, a small sample tissue from endometrial lining (innermost layer of Uterus) is used for evaluating whether the Uterus is ready for implantation of embryo or not.
In the menstrual cycle of a woman the period from 19th to 23rd days is known as “implantation window” during which, the uterus gets prepared for the implantation process. It is part of the luteal phase and the endocrine part of ovaries is producing progesterone. This progesterone brings about modifications in the uterine wall so that, it gets prepared for receiving the embryo. The process involves formation of certain proteins that make the lining thicker and more receptive. In majority of females (84%) this window occurs at the exact time while in very few females (16%) this window occurs either before or after this period.
The IVF treatment in such cases fails as, the embryo transfer is occurring at wrong time. It is happening at the time, when the implantation window is either yet to open or has already been closed. So, the implantation is failing.
When is it prescribed?
It is prescribed in the patients where recurrent implantation failures are observed.
How is it done?
- A small endometrial tissue is collected and expression level of the gene 238 which determines endometrial receptivity is investigated.
- The technique involves assessing RNA levels in different stages of menstrual cycle. As this test is reproducible, its findings remain the same months after and hence, the test is not required to be repeated.
- This investigation can clearly indicate whether this implantation window of a particular woman is happening at the right time or the embryo transfer needs to be scheduled on the different date to match the window so that maturation of endometrial lining can be synchronized with embryo.
What are the advantages?
- Due to precise identification of Implantation Window, embryo transfer can be appropriately planned and can yield assured results.
- The agony of failed transfer can be got rid of.
- A minor shift by one of two days in embryo transfer can result into pregnancy.
Karyotyping
What is it?
Some times, hereditary factors could be responsible for infertility. In such cases before recommending any line of treatment, it is necessary to diagnose the cause of infertility. Studying the genetic or chromosomal composition of the concerned patient to rule out the genetic factor is done in Karyotyping.
PGD (Preimplantation Genetic Diagnosis) involves using one of the embryonic cell for kayotyping. If any defect is detected such embryos can be discarded and healthy embryos can be used for implantation.
Every normal body cell except Red Blood Cells has a set of 46 chromosomes (23 pairs) in its nucleus. These chromosomes are received from both the parents. These can be arranged in 23 pairs out of which the 23rd pair (Sex chromosomes or heterosomes) defines sex of the individual while other 22 pairs (somatic chromosomes or autosomes) of chromosomes define other body characters. Various units of heredity (genes) are located on these chromosomes. In karyotyping technique the integrity of chromosomes can be identified and any aberration in them can be detected. This can give an insight about any congenital abnormality that can result in the child to be born.
How is it done?
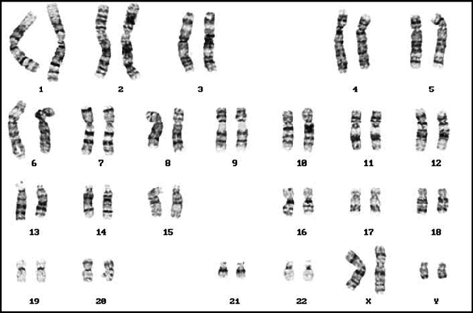
- Venous blood is drawn from concerned patient.
- Cells in the drawn blood are grown in laboratory and are allowed to grow.
- These cells are then stained appropriately and observed under microscope.
- By a specialized technique, it is possible to observe chromosomes from these cells and thus, genetic disorder if any can be diagnosed.
When is it recommended?
Karyotyping is recommended under following conditions so as to define the genetic anomaly and prevent it from being passed on to next generation.
- If the patient is not able to conceive for over year.
- There is a history of still births.
- Miscarriages are reported.
- Primary ovarian dysfunctions such as Primary ovarian insufficiency (POI), Premature Ovarian Failure (POF) are diagnosed as reasons for infertility in female partner.
- Infertility in male partner is found to be due to very few sperms in semen (Oligozoospermea) or absence of sperms in semen (Azoospermea).
What are the advantages?
- If cause of miscarriages is found to be genetic in origin, suitable treatment can be recommended to overcome it.
- By identifying defective genes in the parents, their being into next generation can be avoided.
- There are certain disease-causing genes either of the parents can be carrying. Some of these may be found in both the parents and can result into serious consequences if passed on to the next generation. This can be avoided by carrying out karyotyping of parents. Cystic fibrosis is one such example.
In routine IVF technique, usually a healthy sperm participates in fertilization but, if ICSI is carried out even an unhealthy sperm can be used for fertilization.
