Low Sperm Count
Treatments
- ICSI
- TESA / MESA / PESA / TESE
- MACS
ICSI
What is it?
It is a laboratory procedure where a single sperm is picked up with a fine glass needle and is injected directly into the egg. This is carried out in the laboratory by experienced embryologists using special equipment.
When is it recommended?
It is recommended in any or more of the following conditions.
- When the sperm count is very low
- When the sperm cannot move properly or are in other ways abnormal
- When sperm has been retrieved surgically from the epididymis (MESA/PESA) or the testes
- (TESE/TESA), from urine or following electro-ejaculation
- When there are high levels of antibodies in the semen
- When there has been a previous fertilisation failure using conventional IVF.
What are the advantages?
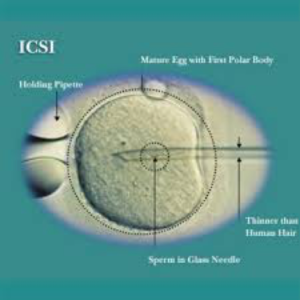 Very few sperms are required for the process and the ability of the sperm to penetrate the egg is no longer important as this has been assisted by the ICSI technique. ICSI does not guarantee that fertilisation will occur as the normal cellular events like fusion of nuclei still need to occur once the sperm has been placed in the egg.
Very few sperms are required for the process and the ability of the sperm to penetrate the egg is no longer important as this has been assisted by the ICSI technique. ICSI does not guarantee that fertilisation will occur as the normal cellular events like fusion of nuclei still need to occur once the sperm has been placed in the egg.
TESA / MESA / PESA / TESE
Testicular Sperm Aspiration / Micro Epididymal Sperm Aspiration / Percutaneous Epididymal Sperm Aspiration / Testicular Sperm Extraction
What is it?
It is a method of drawing sperms directly from Testis or Epididymis with a syringe and needle or by a surgical procedure.
When is it recommended?
When the ejaculate does not contain vital sperms one of these methods is recommended.
How is it performed?
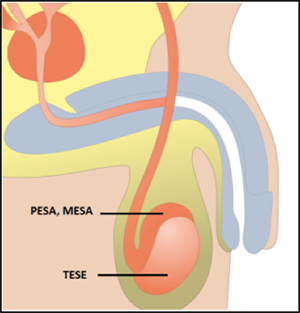 PESA AND MESA involve extraction of sperms from Epididymis (a tubular extension of testis). This is done when the Vas Deferens (duct that carries sperms away from testis for being ejaculated) is impaired. In the event of the PESA method the sperms are aspirated together with the fluid from epididymal ducts with a fine needle directly through the skin of scrotum. In MESA method a small microsurgical skin incision is performed, a puncture needle is inserted via this incision and the fluid is aspirated. The fluid is immediately analyzed in an embryology laboratory.
PESA AND MESA involve extraction of sperms from Epididymis (a tubular extension of testis). This is done when the Vas Deferens (duct that carries sperms away from testis for being ejaculated) is impaired. In the event of the PESA method the sperms are aspirated together with the fluid from epididymal ducts with a fine needle directly through the skin of scrotum. In MESA method a small microsurgical skin incision is performed, a puncture needle is inserted via this incision and the fluid is aspirated. The fluid is immediately analyzed in an embryology laboratory.
TESE
If sperms can not be obtained by MESA method, TESE is performed. In TESE, sperms are obtained directly from the testicular germinal epithelium. Tissue samples are taken from small incisions in the outer testicular layer and are analysed in the embryology laboratory to confirm presence of sperms in the aspirated fluid.
What are the advantages?
- The procedures are performed on the outpatient basis in a short general anesthesia.
- The procedure can be planned for the same day as the oocyte pickup from the female partner.
- The obtained fresh sperms are immediately used for oocyte fertilization with the IVF or ICSI
- The spare tissue is cryopreserved to avoid the need to repeat the procedure.
MACS - Advanced Magnetic Sperm Cell Sorting
What is it?
MACS is a technique which allows the spermatozoa with the best characteristics to be selected for use in Assisted Reproduction Treatments. This technique removes apoptotic (those which will disintegrate without achieving fertilisation) spermatozoa and helps select the healthy ones, thus increasing the possibility of pregnancy.
How is it done?
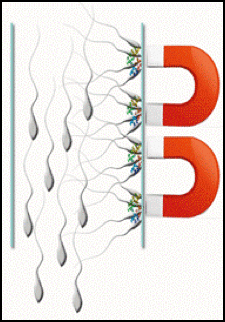
- The semen sample is processed as in normal IVF procedure and collected in small tube.
- Into this tube biodegradable magnetic particles with antibody molecule attached to each are released.
- These magnetic particles attract degenerating sperm cells which remain attached to them.
- A weak magnet is placed next to the tube towards which the weaker spermatozoa get attracted while the healthy sperms move down by gravity. These healthy sperms can be separated and used in suitable ART procedure.
When is it recommended?
This technique can be used with any kind of patient who opts for ART, but is mainly used with:
- Patients who are to be treated with artificial insemination.
- Infertile patients who have a high level of DNA fragmentation in their spermatozoa.
- Patients who have had repeated miscarriages with an unidentified cause.
- Patients who have had at least one previous treatment cycle or who have poor embryo quality which is not attributable to the oocytes.
