Multiple IVF Failure
Treatments
- Endometrial Receptivity Array
- Fertility Surgery
- PGD
- PGS
- Blastocyst Transfer
- ICSI
- Laser Assisted Hatching
- Embryo Glue
- Fertility Booster Diet
- Weight Loss Management
Endometrial Receptivity Array
What is it?
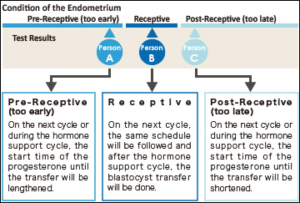 The term ERA stands for Endometrial Receptivity Analysis or Array. In this test, a small sample tissue from endometrial lining (innermost layer of Uterus) is used for evaluating whether the Uterus is ready for implantation of embryo or not.
The term ERA stands for Endometrial Receptivity Analysis or Array. In this test, a small sample tissue from endometrial lining (innermost layer of Uterus) is used for evaluating whether the Uterus is ready for implantation of embryo or not.
In the menstrual cycle of a woman the period from 19th to 23rd days is known as “implantation window” during which, the uterus gets prepared for the implantation process. It is part of the luteal phase and the endocrine part of ovaries is producing progesterone. This progesterone brings about modifications in the uterine wall so that, it gets prepared for receiving the embryo. The process involves formation of certain proteins that make the lining thicker and more receptive. In majority of females (84%) this window occurs at the exact time while in very few females (16%) this window occurs either before or after this period.
The IVF treatment in such cases fails as, the embryo transfer is occurring at wrong time. It is happening at the time, when the implantation window is either yet to open or has already been closed. So, the implantation is failing.
When is it prescribed?
It is prescribed in the patients where recurrent implantation failures are observed.
How is it done?
- A small endometrial tissue is collected and expression level of the gene 238 which determines endometrial receptivity is investigated.
- The technique involves assessing RNA levels in different stages of menstrual cycle. As this test is reproducible, its findings remain the same months after and hence, the test is not required to be repeated.
- This investigation can clearly indicate whether this implantation window of a particular woman is happening at the right time or the embryo transfer needs to be scheduled on the different date to match the window so that maturation of endometrial lining can be synchronized with embryo.
What are the advantages?
- Due to precise identification of Implantation Window, embryo transfer can be appropriately planned and can yield assured results.
- The agony of failed transfer can be got rid of.
- A minor shift by one of two days in embryo transfer can result into pregnancy.
Fertility Surgery
What is it?
A corrective surgery advised for the patients having structural abnormality of reproductive organs so as to improve the chances of conception. It can be for the male or the female partner.
How is it done?
First, minimal invasive diagnostic techniques are used to identify the problem and then a suitable surgical procedure is performed to correct it. The protocol can shortly shown as follows :
Female:
- Reversal of Tubectomy (Tubal ligation). The patient who has already undergone tubectomy for avoiding further pregnancies if decides to have a baby, this kind of surgery can be a solution wherein the ligatured (closed) fallopian tube is reconnected.
- Reconnecting fallopian tube: If there is blockage in fallopian tube due to some infection and pregnancy is not happening because of this, the tube can be reconnected surgically to solve the problem. It involves insertion of a small tube through cervix, uterus and connect the fallopian tube. The surgery is called Salpingostomy, sometimes called neosalpingostomy (the fallopian tube may be cut completely to open the passage for egg cells) or fimbrioplasty (when the tip of fallopian tube that is very close to ovarian is blocked, the tip if surgically opened).
- Polypectomy: A polyp is an abnormal collection of tissue. A polypectomy is a surgical procedure to remove polyps from the from an organ like Uterus. The procedure is relatively noninvasive and is usually carried out at the same time as a hysteroscopy.
- Myomectomy: This procedure sometimes also known as fibroidectomy, refers to surgical removal of uterinefibroids (leiomyomas). In comparison to hysterectomy, the uterus remains preserved in this procedure and the woman retains her reproductive potential.
- Dilatation for treating cervical stenosis: Cervical stenosis means a conditions wherein the cervix becomes extremely narrow. The treatment for this condition is using a dilator.
- Adhesiolysis: Some times, pelvic adhesions are observed blocking passage between uterus and ovarian. In such conditions natural pregnancy becomes difficult and even in ART oocyte pickup is obstructed by the adhesions. This disorder is treated by microsurgical technique or laparoscopic surgery to remove the adhesion and prevent its recurrence.
- Metroplasty: Sometimes, uterus is abnormal in shape such as ‘T’ or heart shaped and hence, can lead to complications during and after pregnancy. This condition is treated with metroplasty. The surgery involves reconstruction of uterine chamber to make into normal shape. With the surgery, implantation of embryo and further development is possible.
- PCO Drilling: Polycystic ovarian can cause the female body produce excess of testosterone and insulin, leading to fertility problems. High testosterone levels can cause irregular menstrual cycles, prevent ovulation and hinder pregnancy. Ovarian drilling can cure this problem Ovarian drilling is a laparoscopic procedure performed under general anesthesia. This surgery is typically done on an outpatient basis with minimal recovery time. With a laparoscopic tool small openings are mad in ovarian.
- Ovarian cystectomy: Endometriomas or chocolate cysts are benign masses growing around ovarian and obliterate the normal process of ovulation. Removal of these cysts is called cystectomy. The surgery needs to be done very carefully as there is a possibility of damage to ovarian vascular supply. Further, there is some decline in ovarian functioning after surgery. So, ART may be necessary for pregnancy.
Male:
- Treat varicocele(swelling of veins coming of Testis) which will allow testes to produce better sperms.
- Removal of blockage in the Epididymis (tubular extension of testis responsible for activation of spermatozoa).
- Reversal of Vasectomy. This is done when the couple decides to go for pregnancy after vasectomy surgery.
- Removal of sperms from testis surgically in case of Azoospermia (Absence of sperms in Ejaculate).
PGD - Pre-implantation Genetic Diagnosis
What is it?
Pre-implantation Genetic Diagnosis is genetic screening technique which allows an expert to examine the genetic composition of a pre-embryo before it is transferred to the patient’s uterus so that, transmission of hereditary disorders into next generation can be avoided.
Why is it recommended?
A normal human genetic code consists of 23 pairs of chromosomes, and each of the chromosomes may contain hundreds of genes. This genetic material is inherited from gametic cells of both mother and father. The combination of these genes creates the character blueprint for the offspring. Unfortunately, the process may not always work seamlessly. Disorders in the chromosomes or particular gene lead to complications in pregnancy or miscarriage or serious genetic diseases. PGD can help in identification of the issues well before the pregnancy occurs.
In an IVF cycle, the embryos are selected using visual criteria: the embryo or embryos that look healthy are chosen for transfer. Sometimes, a visual inspection is not enough. Some serious genetic abnormalities are invisible to the eye. This is where PGD can be used. Following hereditary abnormalities can be identified with PGD:
- Turner’s syndrome.
- Klinefelter’s syndrome.
- Translocation which can cause miscarriages or some forms of leukemia or cancer.
- Cystic fibrosis.
- Tay-Sachs disease.
- Duchenne muscular dystrophy.
- Sickle-cell anemia.
When is it recommended?
PGD can be recommended in following conditions:
- Women age 35 and older because there is a concern about the genetic quality of their eggs.
- Women experiencing recurrent, unexplained pregnancy loss.
- Women with more than one failed fertility treatment.
- Carriers of sex-linked disorders – they can choose gender determination to prevent sex-linked disease.
- Carriers of single gene disorders.
- Couples with family history of inherited disease.
- Those with chromosomal disorders.
What are the advantages?
- Avoids the need for amniocentesis (with a needle and syringe, some amniotic fluid from around the embryo is drawn for pre-natal examination) which be an uncomfortable technique and involves some risk.
- Enables the selection and implantation of healthy pre-embryo resulting into better chances of pregnancy and lower possibility of miscarriage.
- With proper screening fewer embryos are used for transfer thus, minimizing possibility of multiple births.
PGS - Pre-implantation Genetic Screening
What is it?
It is the genetic study of embryo produced during IVF treatment & can help in having a healthy baby. The technique is helpful to identify embryos with the correct number of chromosomes for successful fertility treatment. PGS is performed on the embryo before it is transferred. This allows the identification & transfer of embryos free from any hereditary abnormalities.
When is it recommended?
It is recommended under following conditions:
- If the female partner is more than 35 years.
- The female has suffered 2 or more miscarriages.
- There is history of previous IVF failures.
- Infertility is due to some male factor.
What are the advantages?
- Reduced miscarriage rates.
- Higher pregnancy rate per transfer.
- Greater chances of having a healthy baby.
Blastocyst Transfer
What is it?
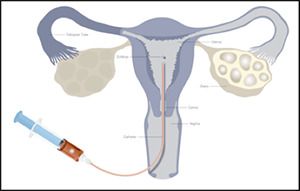
The embryo formation after fertilization involves a number of stages such as 2 cell, 4 cells, 8 cells stage, Morula and so on. Gradually, the cells become distinct as outer cells (Trophoblast) and inner cell mass (embryonic cells). There is a small cavity in between. This stage is called blastocyst. Usually, the protective covering of embryo (Zona Pellucida) is still intact. The blastocyst hatches out of this covering to get implanted into endometrial lining (Innermost covering of uterus).
Using this blastocyst (developed in laboratory) for embryo transfer in IVF technique is called blastocyst transfer (Blast transfer).
When is it recommended?
Blast transfer is recommended for those patients with one more of the following conditions.
- The patients of higher age (35 years or more).
- Repeatedly failed IVF cycles.
- Recipient patients (who are receiving eggs or embryos from donor).
- Those who don’t have the mental preparation for further IVF cycles.
What are the advantages?
- Higher success rates even for patients of higher age.
- Growth pattern of the embryo is established in the laboratory before implantation. So, the doctor has a clear understanding about progress of embryo after implantation.
ICSI
What is it?
It is a laboratory procedure where a single sperm is picked up with a fine glass needle and is injected directly into the egg. This is carried out in the laboratory by experienced embryologists using special equipment.
When is it recommended?
It is recommended in any or more of the following conditions.
- When the sperm count is very low
- When the sperm cannot move properly or are in other ways abnormal
- When sperm has been retrieved surgically from the epididymis (MESA/PESA) or the testes
- (TESE/TESA), from urine or following electro-ejaculation
- When there are high levels of antibodies in the semen
- When there has been a previous fertilisation failure using conventional IVF.
What are the advantages?
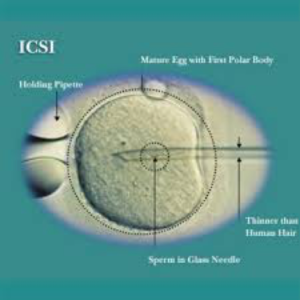 Very few sperms are required for the process and the ability of the sperm to penetrate the egg is no longer important as this has been assisted by the ICSI technique. ICSI does not guarantee that fertilisation will occur as the normal cellular events like fusion of nuclei still need to occur once the sperm has been placed in the egg.
Very few sperms are required for the process and the ability of the sperm to penetrate the egg is no longer important as this has been assisted by the ICSI technique. ICSI does not guarantee that fertilisation will occur as the normal cellular events like fusion of nuclei still need to occur once the sperm has been placed in the egg.
Laser Assisted Hatching
What is it?
An embryo has a protective layer around it (zona pellucida) in early days of development. The process of implantation of the embryo begins on the fifth or sixth day after fertilization, when the embryo leaves its protective shell, zona pellucida disappears and the embryo cells get into direct contact with the cells of uterine wall (endometrium). This also causes elimination of a mechanical barrier which would impede further growth of the embryo.
Laser-assisted hatching: Using a specialized laser to breach the zonapellucida is another possibility. Laser-assisted hatching allows much more control of the size of the hole created. Laser assisted hatching is safest and most effective.
How is it done?

Problems with recurrent implantation failure may be caused by the embryo’s inability to “abandon” its protective shell or by the changes in the protective layer. In such cases, we perform the assisted hatching. In this technique we disrupt the hard shell of the embryo by laser (laser assisted hatching) or by a special needle(assisted hatching), just before the transfer. Thus we make it easier for it to attach to the uterine wall.
How do Embryos hatch naturally?
The oocyte (egg) before fertilisation has a protein-shell surrounding it known as the zona pellucida. The zona pellucida has many functions in embryo development which, change as the embryo grows.
- Before the egg becomes an embryo, the zona pellucida fuses with sperm cells. This is the start of the fertilization process.
- Once a single sperm cell penetrates the shell and fertilizes the egg, the zona pellucida hardens. This prevents more sperm cells from entering the now-fertilized zygote.
- The hardened shell also helps prevent the embryo from implanting prematurely in the fallopian tubes (which would cause an ectopic pregnancy).
- It also keeps the many blastocyst cells together.
- As the zygote travels down the fallopian tube and develops into the blastocysts stage, the zona pellucida expands and begins to thin and deteriorate.
- Around day four of development, the zona pellucida cracks open and the blastocyst/embryo emerges, leaving behind the thin-protein shell. This is the embryo hatching process.
- Within a few days of hatching, the blastocyst implants itself into the endometrium.
When is assisted hatching recommended?
- For older women who have eggs with a harder shell.
- For repeated implantation failure.
- For frozen embryos.
Embryo Glue
What is it?
It is a hyaluronan-enriched medium for embryo transfer (ET) which aids in implantation of embryos and thus, improves pregnancy rates in in-vitro fertilization-ET cycles (IVF-ET).
How is it done?
Eggs are collected in regular medium and IVF is carried out. These are then fertilizes and allowed to develop into embryos. The embryos are allowed to grow till implantation stage and just before implantation, they are then transferred to embryo glue so that, the glue sticks to embryo. Some embryo glue is transferred to endometrium so that the embryo can be fixed onto it.
When is it recommended?
It is recommended in following conditions.
- Repeated failures in IVF cycles after embryo transfer.
- Embryo fails to implant itself after appropriate transfer protocol.
Fertility Booster Diet
Intake of proper food becomes very important during the fertility treatment. Eating certain foods during different phases of your menstrual cycle can enhance the fertility. So, if a woman wants to maximize her chances of conceiving, it is possible to eat foods that have advantageous to each phase. So, we ask our experts to weigh in on what to actually eat during each of the reproductive phase.
The list includes:
1. Plenty of fruits and vegetables
2. Complex carbohydrates – whole grains like brown rice , oats and whole meal bread .
3. Organic food where possible.
4. Oily foods like nuts, fish and oil.
5. Add lemon , pomegranate, green leafy vegetables and tomatoes to diet .
6. Flax seeds + sunflower seeds .
7. Avoid trans fats.
8. Increase intake of fibre.
9. More fish and organic eggs than red meat .
10. Avoid additive ,preservatives and artificial sweetner.
11. Reduce and avoid sugar both on its own and hidden in food .
12. Avoid caffeine : coffee, chocolate ,tea ,cola & alcohol .
13. Avoid processed food.
14. Try having fresh and home-made food.
Weight Loss Management
What is it?
It is avoiding weight gain or losing weight for improving the chances of conceiving. Too low or too high body weight can interfere with fertility of an individual and hence, needs to be managed appropriately.
How is it done?
Normally, weight loss management involved diet and exercise. The couple trying for pregnancy needs to take careful measures in this. Proper diet and moderate exercise are best recommended for weight loss. But during pregnancy if necessary, weight management must be done preferably by diet control. Heavy exercise can affect the embryonic development in uterus and hence, has to be avoided.
When is it recommended?
Excess body weight in female partner is known to reduce the possibility or pregnancy. There is a need to manage the weight appropriately for natural pregnancy or even IVF. When an obese patient approaches for IVF treatment, before treatment the patient needs to undergo weight management regime and only then the IVF protocol can be followed. As mentioned above, the weight loss should be by controlled diet and not entirely by exercise.
